The A1C Test Explained: What Your Blood Says About the Last Three Months
We often think of health checkups as snapshots — a quick look at what’s happening today.
But when it comes to diabetes, what truly matters is the story your blood tells over time.
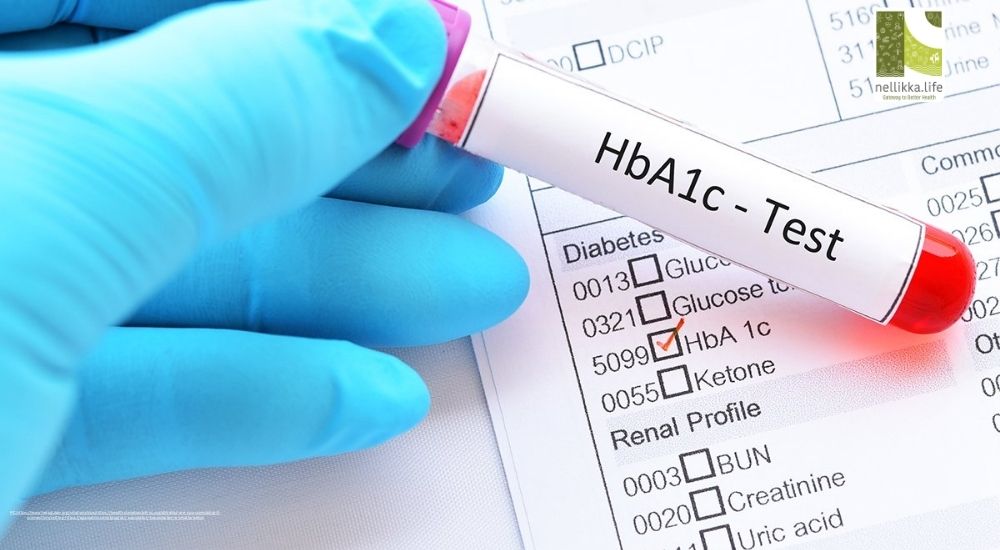
That’s where the A1C test (also known as the HbA1C test) comes in — a small blood test that reveals a big picture: how well your body has been managing sugar levels over the past three months.
At Nellikka.life, we break down the science, the meaning, and the practical wisdom behind this simple but powerful test that helps prevent diabetes complications and keeps your health on track.
What Exactly Is the A1C Test?
The A1C test measures the percentage of glucose (sugar) attached to your red blood cells.
Here’s the logic: red blood cells live for about 120 days (roughly three months). During that time, glucose in your bloodstream naturally sticks to them.
The more sugar in your blood, the more glucose binds to those cells.
The test result — expressed as a percentage — shows how much of your hemoglobin (the oxygen-carrying part of red blood cells) is “glycated” or coated with sugar.
In Simple Terms:
Think of it like checking the average sweetness of your blood over time — not just what’s happening after one meal or fasting.
Understanding Your A1C Numbers
| A1C Result | What It Means | Estimated Average Blood Glucose (mg/dL) |
|---|---|---|
| Below 5.7% | Normal | Below 117 |
| 5.7% – 6.4% | Prediabetes (increased risk) | 117 – 137 |
| 6.5% or higher | Diabetes | 137 and above |
These ranges are based on American Diabetes Association (ADA) guidelines and are used worldwide.
So, if your A1C is 6.8%, it means your average blood sugar has been around 150 mg/dL over the past few months — higher than healthy levels.
Why Doctors Prefer A1C Over a Single Blood Sugar Test
Unlike fasting or post-meal glucose checks, which can fluctuate depending on when or what you eat, the A1C gives a more stable, long-term view.
It reflects your overall glucose exposure and helps your doctor:
- Diagnose diabetes or prediabetes
- Assess how well treatment plans are working
- Adjust medication, diet, or exercise routines
- Predict the risk of long-term complications
In short, it’s your diabetes report card — an honest summary your daily sugar checks can’t always reveal.
Why Keeping A1C in Check Matters
High A1C levels mean excess sugar is constantly circulating in your blood — silently damaging small blood vessels throughout your body.
This can lead to:
- Eye problems (diabetic retinopathy)
- Kidney damage (nephropathy)
- Nerve pain (neuropathy)
- Heart disease and stroke
Studies show that for every 1% reduction in A1C, the risk of complications decreases by about 25–35%.
So even small improvements matter immensely.
How to Lower A1C Naturally (and Sustainably)
The good news? Lowering your A1C doesn’t mean living in deprivation — it means making consistent, mindful choices.
1. Reimagine Your Plate
- Focus on low-glycemic foods — whole grains, lentils, leafy greens.
- Add protein and healthy fats (like nuts, eggs, or fish) to steady blood sugar.
- Cut down refined carbs, sugar-sweetened drinks, and white bread.
2. Move a Little, Every Day
Even a 30-minute brisk walk improves insulin sensitivity.
Muscles act like sponges, using up glucose and lowering A1C naturally.
3. Manage Stress
Cortisol, the stress hormone, can spike blood sugar.
Try deep breathing, yoga, journaling, or mindfulness — tools proven to support both mental and metabolic health.
4. Sleep Right
Less than 7 hours of quality sleep can raise insulin resistance.
Set a bedtime routine that supports recovery and hormonal balance.
5. Consistency Over Perfection
Skipping meals or crash diets can backfire.
Instead, aim for steady habits — because the A1C rewards long-term effort, not overnight change.
Factors That Can Affect A1C Results
While reliable, A1C tests can sometimes be influenced by certain conditions:
- Anemia or blood loss: May make A1C appear lower than it is.
- Kidney disease: Can alter hemoglobin lifespan.
- Pregnancy: A different test may be preferred to monitor gestational diabetes.
- Ethnic variations: Some groups (like South Asians) may naturally have slightly higher A1C values even at similar glucose levels.
That’s why doctors interpret results in context — alongside fasting glucose, lifestyle, and overall health.
A1C for People With Diabetes
If you already have diabetes, the goal isn’t just lowering A1C but doing it safely.
Your doctor might recommend keeping A1C:
- Below 7% for most adults
- Below 6.5% if you’re younger and otherwise healthy
- Below 8% if you’re older or have other conditions
But remember — numbers are guides, not judgments.
The real aim is stable, sustainable control that supports your energy, organs, and peace of mind
Your A1C is more than a lab number — it’s a window into your habits, hormones, and health.
It tells the truth your daily sugars can’t always show — how your body has been coping month after month.
“You can’t manage what you don’t measure — and you can’t heal what you don’t understand.”
So whether you’re living with diabetes, at risk, or simply health-conscious, getting your A1C checked at least twice a year can help you stay ahead of silent damage and take charge of your future.
References
- American Diabetes Association (ADA). Standards of Medical Care in Diabetes, 2024.
- Mayo Clinic. A1C Test: What It Is and What the Results Mean, 2023.
- Centers for Disease Control and Prevention (CDC). Understanding Your A1C, 2022.
- Diabetes Care Journal. Relationship Between A1C Reduction and Complication Risk, 2021.