Restless Legs Syndrome (RLS): When Your Legs Just Can’t Stay Still
That Unsettling Urge to Move
Imagine you’re lying in bed after a long day, ready to rest — but your legs have other plans. They tingle, twitch, and pull with an irresistible urge to move. No matter how much you shift, the sensation returns as soon as you stop.
This isn’t restlessness or anxiety — it’s a neurological condition called Restless Legs Syndrome (RLS), also known as Willis–Ekbom Disease. Though it affects millions worldwide, RLS is often underdiagnosed and misunderstood.
What Exactly Is Restless Legs Syndrome?
Restless Legs Syndrome is a neurological sensorimotor disorder that causes uncomfortable sensations in the legs (and sometimes arms), accompanied by an uncontrollable urge to move them — especially during rest or at night.
These sensations can feel like:
- Creeping or crawling under the skin
- Tingling, itching, or electric shock-like feelings
- Deep ache or pulling sensation
Moving the legs — walking, stretching, or shaking — brings temporary relief.
Key Feature:
The symptoms worsen at night and disrupt sleep, leading to fatigue, poor concentration, and emotional distress.
The Science Behind It
RLS is linked to an imbalance of dopamine, a neurotransmitter that controls muscle movement.
At night, dopamine levels naturally dip — which may explain why RLS intensifies in the evening.
Studies also suggest a connection between RLS and low iron levels in the brain, since iron is crucial for dopamine function.
Other possible triggers:
- Genetic factors (runs in families)
- Nerve damage or peripheral neuropathy
- Pregnancy (usually temporary)
- Chronic diseases like kidney failure or diabetes
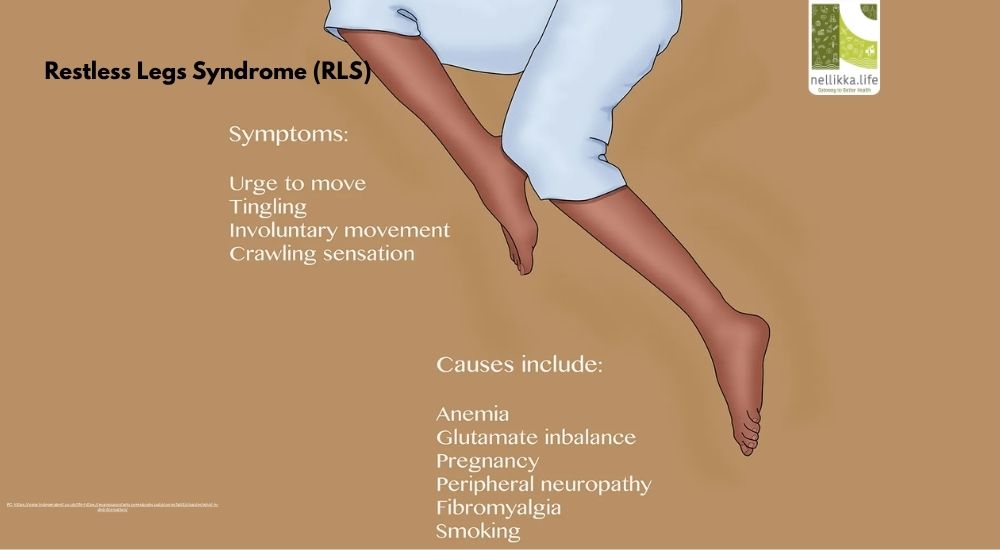
Recognizing the Symptoms
RLS symptoms vary in intensity but share a few hallmark patterns:
- Uncomfortable sensations deep in the legs (rarely in arms)
- Strong urge to move, especially when resting
- Temporary relief when moving
- Worsening during evening or night hours
- Disturbed sleep and daytime fatigue
The International Restless Legs Syndrome Study Group (IRLSSG) outlines these diagnostic criteria.
Common Causes & Risk Factors
1. Primary (Idiopathic) RLS
- Often hereditary, linked to dopamine imbalance.
- Symptoms start before age 40 and can persist lifelong.
2. Secondary RLS
- Triggered by underlying conditions such as:
- Iron deficiency anemia
- Pregnancy (especially in the third trimester)
- Kidney disease
- Diabetes or neuropathy
- Use of certain medications (antihistamines, antidepressants, or antipsychotics)
The Impact on Sleep & Life
RLS isn’t just about leg discomfort — it can severely affect sleep quality.
Many people with RLS experience Periodic Limb Movement Disorder (PLMD) — involuntary jerks during sleep that repeatedly wake them up.
Long-term effects include:
- Chronic sleep deprivation
- Low mood or irritability
- Difficulty focusing at work
- Increased risk of depression and anxiety
Managing Restless Legs Syndrome
Lifestyle Modifications
Small daily habits can help manage symptoms:
- Maintain sleep hygiene: Sleep and wake up at consistent times.
- Stretch and massage: Gentle stretching before bed improves circulation.
- Avoid triggers: Reduce caffeine, nicotine, and alcohol.
- Exercise moderately: Regular walking or yoga helps, but avoid overexertion.
- Warm baths or heating pads: Relaxes muscles before bedtime.
Nutrition Support
- Eat iron-rich foods (spinach, beans, red meat, dates).
- Supplement iron, folate, or magnesium if advised by your doctor.
- Stay hydrated throughout the day.
Medical Treatment
If lifestyle changes aren’t enough, your doctor may prescribe:
- Dopamine agonists (pramipexole, ropinirole)
- Iron supplements (if deficiency is found)
- Anti-seizure medications (gabapentin, pregabalin)
- Sleep aids or mild sedatives (in severe cases)
RLS and the Mind–Body Connection
RLS is often worse with stress and anxiety. Relaxation techniques such as:
- Deep breathing
- Meditation
- Gentle yoga
- Aromatherapy (lavender, chamomile)
help calm the nervous system, improving both sleep and symptoms.
When to See a Doctor
Seek medical advice if:
- Your symptoms disrupt sleep more than 3 nights a week
- You have persistent tiredness or low energy
- You notice symptoms spreading to arms or worsening over time
A simple blood test for iron levels and a sleep assessment can identify treatable causes.
Restless Legs Syndrome isn’t “all in your head.” It’s a real, treatable neurological disorder that can profoundly impact quality of life.
By addressing underlying causes, improving sleep habits, and working with healthcare professionals, most people can find lasting relief.
Your legs deserve rest — and so do you.
References
- National Institute of Neurological Disorders and Stroke (NINDS): Restless Legs Syndrome Fact Sheet, 2024
- American Academy of Sleep Medicine (AASM): Clinical Practice Guidelines for RLS, 2023
- Mayo Clinic: Restless Legs Syndrome — Causes and Treatment, 2024
- Sleep Medicine Journal, 2022: Iron Deficiency and Dopaminergic Pathways in RLS





