Pericarditis: When the Heart’s Shield Turns Against Itself
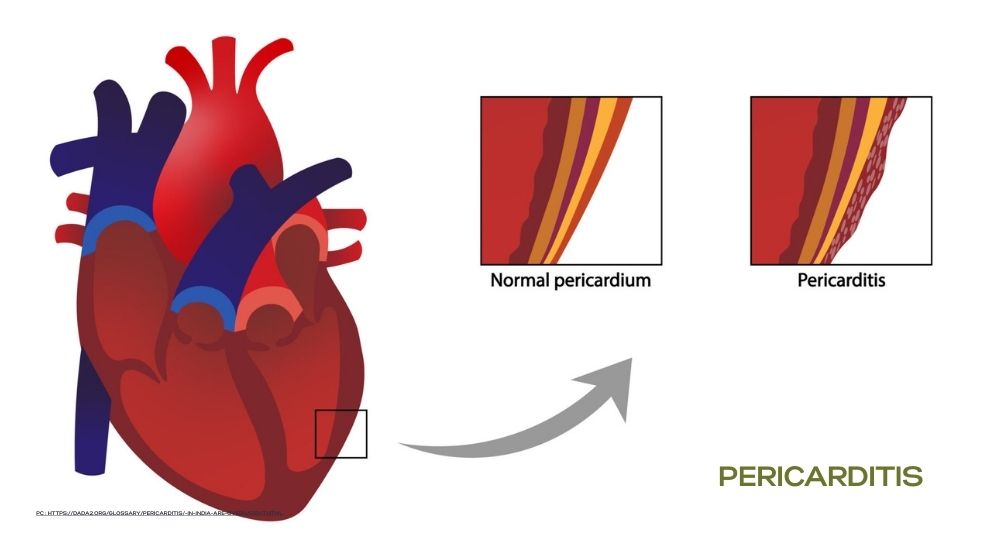
Understanding the Heart’s Protective Layer
Your heart isn’t just a powerful muscle — it’s also protected by a thin, double-layered membrane called the pericardium.
This sac cushions the heart, keeps it in place, and prevents friction as it beats over 100,000 times a day.
When this protective covering becomes inflamed, the condition is called Pericarditis — and while it’s often temporary, in some cases it can cause severe pain or even complications that affect heart function.
What Is Pericarditis?
Pericarditis is an inflammation of the pericardium, often triggered by an infection or immune response.
It can occur suddenly (acute) or develop slowly (chronic).
The inflammation causes the layers of the pericardium to rub against each other, resulting in sharp chest pain that may mimic a heart attack.
Types of Pericarditis
- Acute Pericarditis
Sudden onset; usually resolves within a few weeks. - Recurrent Pericarditis
Symptoms return after a symptom-free period. - Chronic Pericarditis
Long-lasting inflammation that may lead to scarring and thickening of the pericardium. - Constrictive Pericarditis
Severe, chronic form where the pericardium becomes stiff and restricts the heart’s ability to pump blood effectively.
What Causes Pericarditis?
Pericarditis can have many triggers, but in many cases, the exact cause remains unknown (idiopathic).
Common causes include:
- Viral infections (Coxsackievirus, Influenza, COVID-19)
- Bacterial infections, including tuberculosis (especially in India)
- Autoimmune diseases (Rheumatoid arthritis, Lupus)
- Heart attack or cardiac surgery (post-myocardial infarction pericarditis)
- Kidney failure (uremic pericarditis)
- Certain medications or radiation therapy
- Chest injury or trauma
Common Symptoms
The hallmark symptom is sharp, stabbing chest pain that:
- Often worsens when lying down or taking a deep breath
- Improves when sitting up and leaning forward
Other symptoms include:
- Fever and fatigue
- Shortness of breath
- Heart palpitations
- Dry cough
- Swelling in legs or abdomen (in chronic cases)
Pericarditis pain can sometimes feel similar to a heart attack — always seek immediate medical attention if in doubt.
How Is It Diagnosed?
Diagnosis involves a combination of clinical evaluation, imaging, and blood tests:
- Physical Examination:
A doctor may hear a distinctive “pericardial friction rub” using a stethoscope — a telltale sign. - ECG (Electrocardiogram):
Shows changes distinct from those in heart attacks. - Echocardiogram:
Detects pericardial fluid (effusion) or thickening. - Chest X-ray or CT/MRI:
Reveals enlarged cardiac silhouette or inflammation. - Blood Tests:
Elevated ESR, CRP, or troponin levels confirm inflammation.
Treatment: Relieving the Pressure on the Heart
Most cases of acute pericarditis resolve with timely treatment.
The goal is to reduce inflammation and treat the underlying cause.
Typical treatments include:
- Anti-inflammatory medications (NSAIDs or colchicine)
- Corticosteroids (for autoimmune or recurrent cases)
- Antibiotics or anti-tubercular therapy (if bacterial or TB-related)
- Drainage of excess pericardial fluid (pericardiocentesis) if it causes compression on the heart — a condition known as cardiac tamponade
Early treatment usually results in full recovery within a few weeks.
Possible Complications
If left untreated or recurrent, pericarditis can lead to:
- Pericardial effusion (fluid buildup around the heart)
- Cardiac tamponade (life-threatening compression)
- Constrictive pericarditis (scarring and stiffening of the pericardium)
Prevention & Lifestyle Support
While not all cases can be prevented, you can reduce your risk by:
- Managing infections promptly
- Controlling autoimmune or chronic conditions
- Avoiding self-medication with unprescribed drugs
- Following up regularly after heart surgery or heart attack
Heart-Healthy Habits Help Too:
- Eat anti-inflammatory foods (omega-3s, greens, turmeric, fruits)
- Avoid smoking and alcohol
- Practice gentle yoga and breathing techniques for stress control
Listen to What Your Heart Says — Literally
Pericarditis might be rare, but its symptoms can be mistaken for something less serious — or something far worse.
The key is awareness.
If you experience persistent chest pain, fever, or shortness of breath, don’t wait.
Consult a cardiologist or reach out to Nellikka’s heart wellness panel for guidance and screening.
Your heart speaks through discomfort — listen before it cries for help.