Migraines vs Tension Headaches: How to Tell the Difference
Headaches are among the most common health complaints worldwide — yet they are also among the most misunderstood. Many people casually label every headache as a “migraine,” while others ignore recurring pain as simple stress. In reality, migraines and tension headaches are distinct neurological experiences, with different causes, patterns, and management approaches.
Understanding the difference is not just about naming the pain correctly. It is about listening to what the body and brain are trying to communicate — and responding in a way that prevents long-term suffering.
Why Differentiating Headaches Matters
Treating all headaches the same often leads to:
- Inadequate relief
- Overuse of painkillers
- Worsening frequency and intensity
- Missed underlying triggers
Migraines, in particular, are not “severe headaches” — they are a complex neurological condition involving the brain, blood vessels, nerves, hormones, and sensory processing.
Tension headaches, on the other hand, are closely linked to muscle tension, stress, posture, and emotional load.
Knowing which one you experience is the first step toward effective relief.
Tension Headaches: The Weight of Stress
What a tension headache feels like
Tension headaches are the most common type of headache. They are often described as:
- A dull, aching pain
- A tight band or pressure around the head
- Heaviness in the forehead, temples, or back of the head
- Neck and shoulder stiffness
The pain is usually bilateral (on both sides of the head) and remains mild to moderate in intensity.
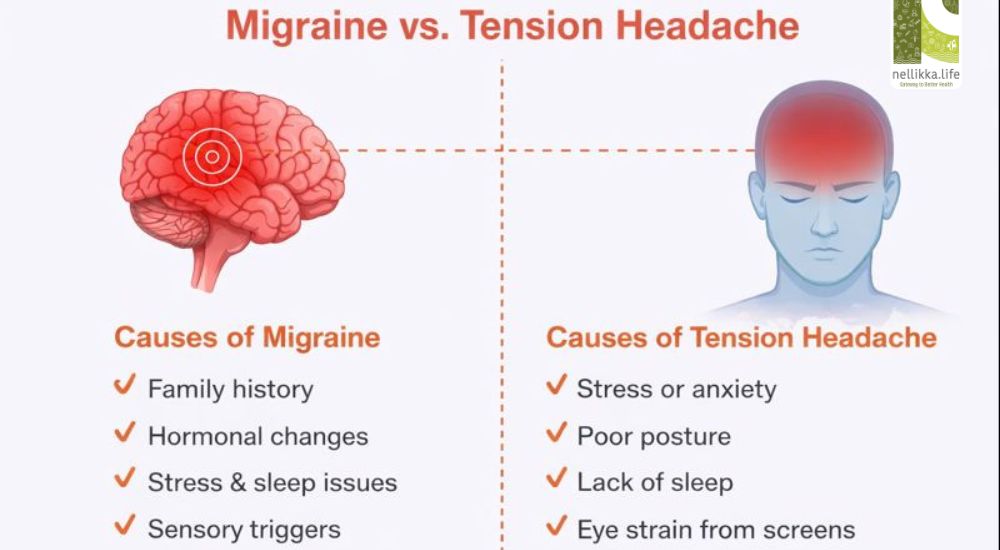
Common triggers of tension headaches
Tension headaches are strongly linked to lifestyle and emotional factors:
- Chronic stress or anxiety
- Long hours of screen use
- Poor posture and neck strain
- Jaw clenching or teeth grinding
- Irregular sleep patterns
- Mental overload and suppressed emotions
These headaches often build up gradually and may persist for hours or days.
Associated symptoms
Tension headaches usually do not cause:
- Nausea or vomiting
- Visual disturbances
- Sensitivity to light or sound
Physical activity does not typically worsen the pain.
Migraines: A Neurological Storm
What a migraine feels like
Migraines are intense and often disabling. They are commonly described as:
- Throbbing or pulsating pain
- Moderate to severe intensity
- Pain on one side of the head (though it can shift)
- Pain that worsens with movement
A migraine is not just head pain — it is a whole-body neurological event.
Key migraine symptoms
Migraines often come with one or more of the following:
- Nausea or vomiting
- Sensitivity to light, sound, or smell
- Visual disturbances (aura) such as flashing lights or zigzag patterns
- Dizziness or vertigo
- Fatigue and brain fog before or after the attack
Some people experience warning signs hours or days before the headache begins, including mood changes, food cravings, or neck stiffness.
Common migraine triggers
Migraine triggers vary from person to person but commonly include:
- Hormonal fluctuations (especially in women)
- Skipped meals or low blood sugar
- Sleep deprivation or oversleeping
- Certain foods (aged cheese, processed foods, excess caffeine)
- Bright lights or loud sounds
- Weather changes
- Emotional stress followed by relaxation
Unlike tension headaches, migraines often have specific neurological triggers.
Key Differences at a Glance
Pain quality
- Tension headache: Dull, tight, pressure-like
- Migraine: Throbbing, pulsating
Pain location
- Tension headache: Both sides of the head
- Migraine: Often one-sided
Intensity
- Tension headache: Mild to moderate
- Migraine: Moderate to severe, sometimes disabling
Associated symptoms
- Tension headache: Neck stiffness, scalp tenderness
- Migraine: Nausea, vomiting, light and sound sensitivity, aura
Effect of activity
- Tension headache: Usually unchanged
- Migraine: Worsens with physical activity
Why Migraines Are Often Misunderstood
Migraines are frequently dismissed as:
- “Just stress”
- “Hormonal issues”
- “Weak tolerance to pain”
In reality, migraine brains are more sensitive to sensory input. They process light, sound, and pain differently. This heightened sensitivity is neurological, not psychological.
Repeated untreated migraines can lead to:
- Increased attack frequency
- Central sensitization
- Medication-overuse headaches
- Reduced quality of life
Early recognition and appropriate management are crucial.
Lifestyle Links: What Both Headaches Have in Common
While migraines and tension headaches are different, they often share underlying lifestyle contributors:
- Poor sleep quality
- Chronic stress
- Irregular eating patterns
- Dehydration
- Excess screen time
- Lack of restorative movement
Modern lifestyles place enormous strain on the nervous system, making headaches more frequent and severe.
Can Headaches Be Prevented?
The good news is that both types of headaches are highly responsive to lifestyle correction.
For tension headaches
- Improve posture and ergonomics
- Take regular screen breaks
- Practice neck and shoulder stretches
- Learn stress regulation techniques
- Prioritize rest and emotional expression
For migraines
- Maintain regular sleep and meal timings
- Identify and avoid personal triggers
- Stabilize blood sugar
- Manage hormonal health
- Practice nervous system calming techniques such as meditation and pranayama
Painkillers may provide temporary relief, but they do not address root causes.
When to Seek Medical Help
Consult a healthcare professional if:
- Headaches are increasing in frequency or severity
- Pain is sudden, severe, or different from usual patterns
- Headaches interfere with daily functioning
- There are neurological symptoms like weakness, vision loss, or confusion
Proper diagnosis helps prevent unnecessary suffering.
Nellikka Perspective: Pain as a Signal
At nellikka.life, headaches are viewed not merely as symptoms to suppress, but as signals from an overworked nervous system.
Migraines ask for sensitivity, rhythm, and internal balance.
Tension headaches ask for rest, release, and emotional honesty.
When we stop fighting pain and start understanding it, healing becomes possible.
Not all headaches are the same.
Listening carefully to the quality of pain reveals its message.
And clarity begins when we respond with awareness rather than endurance.