Childhood Leukaemia: Now Is the Time for Precision Oncology

In today’s medical landscape, we are witnessing extraordinary advancements in how we treat diseases — and nowhere is this more evident than in the field of paediatric oncology. Among the most serious conditions affecting children is leukaemia, or blood cancer. While chemotherapy remains a long-standing and proven treatment, modern medicine is now moving toward more targeted and personalised approaches.
In this article, Dr. Raghu K S, Paediatric Oncologist at Tata Medical Institute, Kolkata, shares key insights on how precision oncology is reshaping the way we treat childhood leukaemia — offering hope, accuracy, and improved outcomes.
The Shift Beyond Traditional Chemotherapy
For years, chemotherapy has been the mainstay in treating childhood leukaemia. While effective, it often comes with significant side effects and a one-size-fits-all approach. Fortunately, we are now in an era where scientific innovation has opened the door to new and more precise treatment options.
Two of the most promising approaches today are:
1. Targeted Therapy
Cancer is fundamentally a genetic disease, caused by specific mutations in cells. Targeted therapy is designed to identify and attack those exact mutations, leaving healthy cells relatively unharmed.
This approach not only increases the chances of remission but also reduces the risk of harmful side effects compared to conventional therapies.
2. Immunotherapy
Immunotherapy uses the body’s own immune system to fight cancer. By stimulating or engineering the immune response, doctors can retrain immune cells to recognise and destroy cancer cells.
This is particularly transformative in paediatric care — where children’s immune systems can be guided to effectively attack leukaemia cells. It’s already proving remarkably successful in high-risk and relapsed cases.
Why Precision Oncology Is the Future
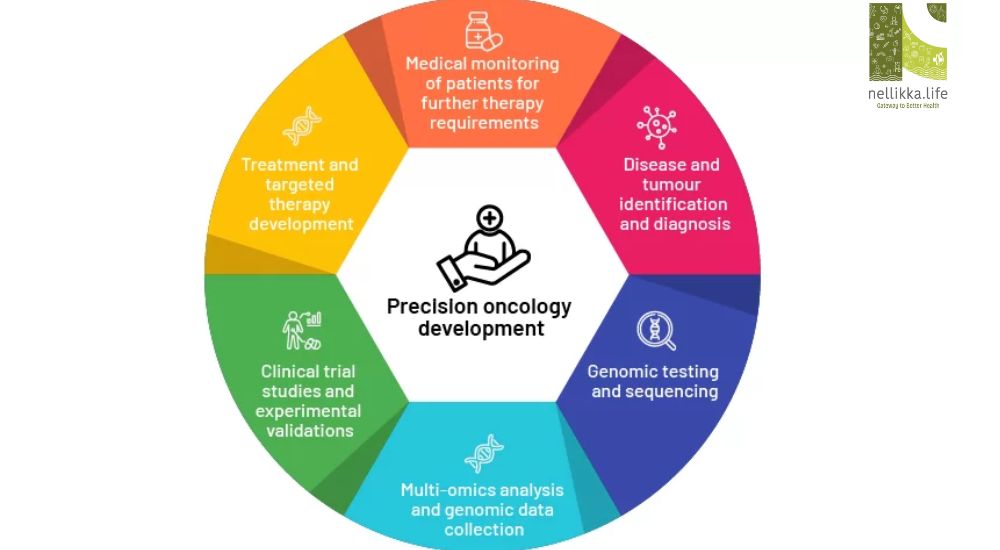
The field of precision oncology focuses on treating every child not just based on their disease, but on their unique genetic profile, disease characteristics, and environment.
This highly individualised approach involves:
- Understanding the genetic mutation causing the cancer
- Analysing the tumour’s molecular behaviour
- Considering the child’s body type, lifestyle, and environment
- Choosing the right drug, for the right child, at the right time
Doctors often conduct genomic testing to identify specific mutations. Once pinpointed, they can use precision drugs that target only those cancer-driving mutations — maximising impact and minimising harm.
The Impact on Childhood Leukaemia
These advancements mark a revolutionary turning point in paediatric leukaemia care. Precision oncology and immunotherapy are not just theoretical — they are already improving survival rates, reducing relapse, and enhancing quality of life for many young patients.
We are entering a future where treatment is less about protocols and more about people — tailored, thoughtful, and precise.