Brittle Truth: Understanding Osteoporosis Before It Breaks You
Imagine your bones as a living, breathing architecture — constantly breaking down old cells and rebuilding new ones. But what happens when that balance tips? When your body starts losing bone faster than it can replace it? That’s the quiet danger called Osteoporosis — often invisible until the first painful fracture.
At Nellikka.life, we break down what osteoporosis really is, why it’s far more common than you think, and how to protect your skeletal foundation before it gives way.
What Exactly Is Osteoporosis?
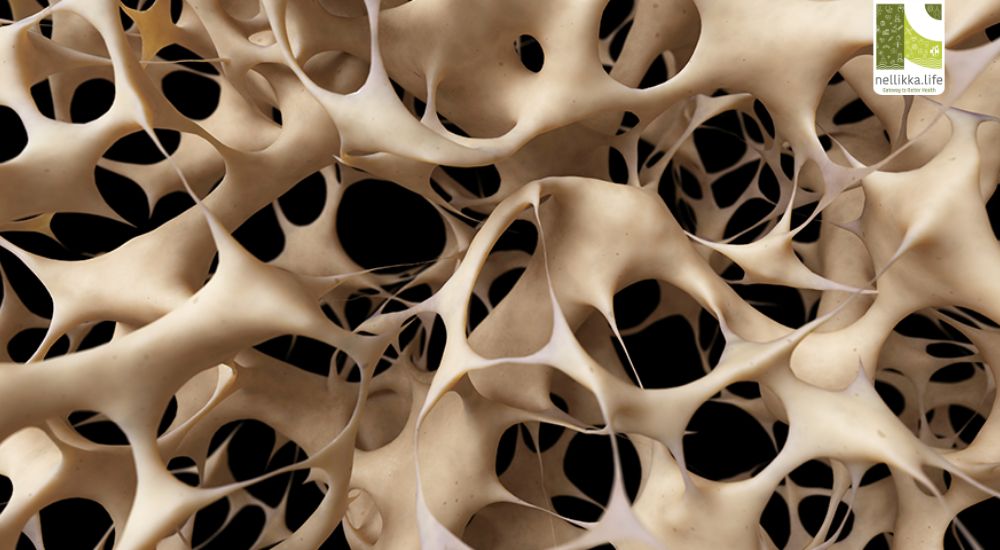
Osteoporosis literally means “porous bone.” It’s a chronic metabolic bone disorder in which bone density and quality deteriorate, making bones fragile and more likely to fracture.
Think of your bone tissue as a honeycomb structure — in healthy bones, the spaces are small and tight. In osteoporosis, those spaces grow larger, weakening the framework.
Common fracture sites include the hip, wrist, and spine, which can drastically reduce mobility and independence, especially in older adults.
The Science Behind Bone Density
Bone is not static; it’s a dynamic tissue that constantly undergoes remodeling — a balance between:
- Osteoclasts that break down old bone, and
- Osteoblasts that build new bone.
In youth, this process favors bone formation. But after age 30, the scale starts to tip, especially in postmenopausal women, when estrogen — a hormone crucial for bone strength — drops sharply.
According to the World Health Organization (WHO), bone mineral density (BMD) is used to diagnose osteoporosis using a DEXA scan (Dual-energy X-ray absorptiometry):
- Normal: T-score above -1
- Osteopenia (mild bone loss): T-score between -1 and -2.5
- Osteoporosis: T-score below -2.5
Why Women Are at Greater Risk
Women are four times more likely than men to develop osteoporosis due to:
- Menopause-related estrogen loss
- Smaller bone mass and density
- Pregnancy and breastfeeding–related calcium shifts
- Diet and lifestyle factors
However, men aren’t immune — particularly those with low testosterone, chronic steroid use, or sedentary lifestyles.
Hidden Risk Factors You Might Miss
Osteoporosis isn’t just about aging. Modern lifestyle plays a silent role.
Risk factors include:
- Nutritional deficiencies: Low calcium, vitamin D, magnesium, and protein
- Sedentary habits: Lack of weight-bearing exercise
- Smoking and alcohol: Both interfere with bone formation
- Caffeine and soda: Excess intake increases calcium loss
- Medications: Long-term use of corticosteroids, PPIs, or certain anti-seizure drugs
- Medical conditions: Thyroid disorders, celiac disease, rheumatoid arthritis
The Role of Vitamin D — The Sunshine Hormone
In India, paradoxically, vitamin D deficiency is rampant despite abundant sunlight. Urban indoor lifestyles, pollution, and use of sunscreens block UVB rays required for vitamin D synthesis.
This deficiency impairs calcium absorption — weakening bones even in calcium-rich diets.
A simple blood test (25-hydroxyvitamin D) can help you track your levels.
Building Strong Bones: What You Can Do
1. Nourish Your Skeleton
- Calcium: 1000–1200 mg/day from milk, ragi, leafy greens, tofu, sesame, or fortified foods.
- Vitamin D: 600–800 IU/day; aim for safe morning sunlight (10–15 min daily).
- Protein: Essential for bone matrix; include lentils, eggs, fish, and nuts.
- Micronutrients: Magnesium, zinc, and vitamin K support bone metabolism.
2. Move for Bone Health
- Weight-bearing exercises like walking, jogging, stair climbing, and dancing improve density.
- Resistance training (with weights or bands) enhances muscle strength and bone remodeling.
- Balance and posture exercises like yoga or tai chi reduce fall risks.
3. Lifestyle Shifts
- Limit caffeine and alcohol.
- Quit smoking — nicotine impairs bone-forming cells.
- Maintain a healthy BMI (underweight individuals are at higher risk).
4. Regular Screening
Especially for:
- Women above 45
- Men above 60
- Anyone with history of fractures, long-term medication use, or family history of osteoporosis.
Medical Management
Doctors may prescribe:
- Bisphosphonates (e.g., alendronate, risedronate) to reduce bone breakdown
- Selective Estrogen Receptor Modulators (SERMs) like raloxifene
- Hormone therapy in postmenopausal women (after risk assessment)
- Calcium and Vitamin D supplements
- Newer biologics such as denosumab or teriparatide for severe cases
Treatment is always individualized — under medical supervision.
Osteoporosis and the Indian Reality
In India, 1 in 3 women and 1 in 5 men over 50 suffer from osteoporosis or osteopenia.
Poor diet, lack of awareness, and cultural neglect of physical fitness accelerate the crisis.
Fractures among older adults often lead to loss of independence or even early mortality — but early intervention can prevent this.
Prevention Is Your Best Medicine
Your bones carry you through every step of life — until you stop carrying them well.
Osteoporosis doesn’t happen overnight, but its prevention starts early. Whether you’re a 25-year-old woman, a 40-year-old office worker, or a 60-year-old retiree — every day you move, eat, and care for your body shapes your skeletal destiny.
At Nellikka.life, we remind you — your bone health is not just about strength; it’s about freedom.
References (Authentic Sources)
- Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO Technical Report Series 843, 1994.
- International Osteoporosis Foundation (IOF)
- National Institutes of Health (NIH) Osteoporosis and Related Bone Diseases Resource Center.
- Kanis JA et al. Diagnosis of osteoporosis and assessment of fracture risk. The Lancet, 2020.